This page is designed to provide an explanation of cough hypersensitivity
If you would prefer to have an offline version you can access and save that here.
Over one in ten people in the UK will suffer from chronic cough and up to 40% of these cases will not respond to medical management1. Intervention from a Speech and Language Therapist has potential to reduce the severity and frequency of coughing episodes.
What is a cough/ cough hypersensitivity?
When we cough, the vocal cords in our voice box clash together creating a burst of air. A cough is meant to:
- Stop harmful material entering the airway, i.e. smoke, mucus, food, etc
- To eject mucus produced in the lungs, i.e. a chest infection.
Cough hypersensitivity is when a cough is triggered in response to a harmless trigger or irritation., e.g., cold air. This is sometimes called laryngeal hypersensitivity (see separate hand out). Cough hypersensitivity is due to abnormal function of the nerves in the airway (throat and lungs) and the parts of the brain that stop a cough.
Cough hypersensitivity can only be diagnosed after other medical professionals have investigated other conditions that may be contributing to your cough, i.e. asthma, COPD, disordered breathing pattern, medications.
Consequences of constant coughing
Coughing itself can develop into a vicious cycle. Once you cough, you may feel the need to take a deep breath, opening your mouth wide to do so. Gasping in this cold and/or dry air can trigger another cough and the cycle continues.
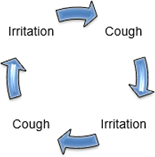
The force of the vocal cords clashing together can also cause more irritation to the lining of the throat making them more sensitive.
The video below demonstrates how much trauma a cough can cause in the throat.
The two white lines sitting in a V-shape at rest are the vocal cords, the space between them is the airway.
Impact of coughing
Some people with cough hypersensitivity say it is unpleasant and can be isolating. For some It can lead to poor sleep, disordered breathing, loss of bladder control, anxiety, isolation and hoarse voice.
Cough control
- 1. Identify what triggers it. With cough hypersensitivity triggers are typically things that don’t make people cough. Common triggers include:
|
Talking |
Aerosols |
Feeling of excess mucus in the throat |
Exercise (usually more effortful) |
|
Laughing |
Perfumes |
Dryness in the throat |
Feeling stressed |
|
Yawning |
Smoke |
Feeling of a tickle in the throat |
Feeling anxious |
|
Taking a deep breath |
Chemicals |
Feeling of a lump in the throat |
Feeling upset or nervous |
|
Shouting |
Strong smells |
Changing head or neck position |
|
|
|
Cold air |
Feeling of acid reflux and/or crumbs in the throat |
|
Some people can find it difficult to identify triggers, particularly if they overlap, or change over time.
2. Identify signs that your cough is about to start. It is helpful to look out for signs of the cough e.g. a tickle or tightness in the throat. This is your cue (or prompt) to start using your cough control breathing exercises which your SLT will go through with you.
3. Make sure your throat is as healthy as possible: It can be more difficult to control cough if the lining of your upper airway (including mouth and throat) is dry. There are a number of things that can be done to improve throat care.
4. Reduce muscle tension in your throat, jaw, tongue and neck: It can be more difficult to control cough if the muscles in our throat and neck are tight. Muscle tension restricts the movement of muscles, making it more difficult to open up the airway and improve breathing. Your SLT will be able to offer advice on the best exercises to release throat tension and tongue/jaw tension. Improving whole body breathing patterns can also help to reduce tension in the upper body.
5. Learn emergency breathing strategies: Some people try to avoid cough triggers, but this is not always possible, especially outside of your own home. We recommend developing techniques to control your breathing if you do come into contact with triggers. These exercises can help to prevent a coughing episode from happening, or make a coughing episode shorter and/or less severe. You will work with your SLT to find emergency breathing techniques that prevent your vocal cords from squeezing together, making it easier to breathe. The most commonly used technique is ‘sniff puff puff’.
Examples of how to manage different triggers
If external irritants are a trigger, it can be helpful to start your breathing exercises BEFORE you come into contact with the trigger. For example, if you are about to walk outside into cold air, you could start your breathing exercises before you get outside. In some cases this isn’t possible (or you might forget) and your cough symptoms could start without warning. In these cases, start your breathing exercises as soon as possible to ‘get you out of the coughing episode’. This aims to make the coughing episode shorter and less severe.
If internal irritants are a trigger, e.g., mucus in the throat, you could focus on improving your hydration and throat care to make the mucus thinner and less irritating. You could also work on changing how your throat muscles respond to the sensation of an irritation e.g., by swallowing mucus and taking gentle breaths in and out through the nose, rather than throat clearing or breath holding.
If voice use is a trigger, you can work on breathing patterns, voice exercises and/or personalised throat relaxation exercises. These help to improve how well the muscles around your lungs coordinate with the muscles in your voice box.
If exercise is a trigger, you can work on introducing helpful breathing patterns, and personalised breathing exercises. It can be beneficial to introduce these before you reach the most challenging point of exercise. You can also work on pacing your exercise.
If emotions are a trigger, your SLT would work with you to explore any unhelpful thinking patterns that may be driving throat tension. You would work together to find different ways to support your wellbeing, and identify the most helpful breathing exercises. Emotions could be specifically related to cough e.g. the fear of being unable to breathe or beliefs about what other people think about your cough. It is however possible for emotions about ‘non-cough related factors’ to affect throat muscles and make them more likely to tighten up.
Cough distraction
- Remind yourself there is no functional benefit to the cough; break the cycle!
- Take a sip of water before the cough happens; this keeps the throat moist.
- Hard/ dry swallow several times; this can help to swallow away any mucus.
- Sniff Puff Puff- take a sharp sniff through your nose and blow out twice through pursed lips.
- Pursed lip breathing; breathe in gently through your nose, then purse your lips making them into a narrow ‘O’ shape and blow out, as if trying to whistle or blow out candles, focus on trying to make the ‘out’ breath longer. This relaxes the throat muscles.
Practice cough control techniques regularly, even when you are not coughing. This will help you retrain your throat muscles so you can use the strategies effectively when you feel the urge to cough or stop a coughing episode.
Our lead respiratory speech and language therapist created this useful video resource on hypersensitive cough in collaboration with Newcastle Hospitals that demonstrate the above cough suppression techniques.
It can be accessed here.
Top tips for throat care
1. Reduce irritation
| Ensure you are well hydrated: |
| Drink 1.5 to 2 litres of water each day, unless advised otherwise by your Doctor. |
| Carry a water bottle at all times for regular sips of wate. |
|
Avoid caffeinated/ alcoholic drinks. |
|
Manage any sinus problems, eg, by using a saline sinus rinse |
| Manage any acid reflux or heartburn |
2. Steam Inhalation (aim for 8-10 times per day):
|
Inhale the steam from a cup of your favourite caffeine free hot drink/ cup of boiling water. |
|
Breath shower steam when having a shower. |
|
Run hot water into a sink or basin and inhale the steam. |
|
Run a washcloth under hot water, wring it out, and hold it near your mouth and nose and breathe in. |
|
Try using a steam inhaler cup. |
3. Medication
|
Some medications have a drying effect on the throat, use steam to combat this. |
|
Rinse your mouth out and steam before and after using powdered inhalers. |
|
Use a spacer with your inhalers if you can. |
|
Ask your medical team if there are any alternative medications, that are less drying in the throat. |
