One of the largest units in the region for colorectal surgery services
Our colorectal service can provide you with specialist treatment for intestinal, bowel or continence problems. This includes colorectal cancer, inflammatory bowel disease (IBD) and pelvic floor conditions.
As one of the largest units in the region for colorectal surgery, we specialise in laparoscopic (keyhole) surgery, which is less invasive and offers a quicker recovery time. You're in safe hands as many of our surgeons are national trainers in laparoscopic colorectal surgery.
Depending on your condition, we can provide dedicated clinics for many lower gastrointestinal symptoms such as change in bowel habit, rectal bleeding, inflammatory bowel disease, constipation and faecal incontinence so the team have expertise in your particular condition.
We place a lot of emphasis on your recovery, and even before any surgery a dedicated enhanced recovery nurse will start to work with you to plan how to get you back to full health as quickly as possible.
If you need a stoma after your treatment, a specialist stoma care nurse will support you during your stay in hospital, and this support will continue once you have returned home.
Our team works closely with other health professionals who may be involved in your care. This includes radiologists, oncologists and histopathologists. This helps ensure the best possible treatment for you.
Clinics, as well as endoscopy, are run from our general hospitals at North Tyneside, Wansbeck and Hexham as well as Alnwick, Berwick and Blyth hospitals, Morpeth NHS Centre and Monkseaton Medical Centre.
Meet our colorectal team
Get to know the members of our colorectal team by clicking the headings below.
Mr Benjamin Box

I have been a Consultant Colorectal Surgeon since 2009. My specialist interests include Inflammatory Bowel Disease, Transanal Minimally Invasive Surgery and Robotic Surgery. I perform lower GI endoscopy.
I have completed a fellowship in Cleveland Clinic, Ohio, United States.
I also have a keen interest in emergency surgery. I was on the ACPGBI emergency general surgery subcommittee and am currently the lead for the National Emergency Laparotomy Audit in the department.
Mr Chris Emmett

I have been a Consultant Surgeon at Northumbria since 2020. My specialist interests include Benign Colorectal Conditions, Colorectal Cancer, Pelvic Floor, Robotic Surgery and Proctology. I perform lower GI endoscopy.
I have completed a PhD in Functional Bowel with Professor Yiannakou in Durham.
I am the Pelvic Floor Lead.
Mr Gareth Hicks

I was appointed as Consultant Surgeon in Northumbria in 2018. My specialist interests include Colorectal Cancer, Pelvic Floor, Robotic Surgery and Proctology. I perform lower GI endoscopy.
I completed a fellowship in pelvic floor at St Peter's Hospital in Surrey.
I am the emergency surgery lead.
Mr Graham O’Dair

I was appointed as a consultant colorectal surgeon in 2009 and have worked in Northumbria since 2020. I have performed major colorectal surgical treatments for conditions including cancer and benign disorders with minimally invasive surgery (keyhole) for all this time and with robotic-assisted surgery since 2017.
I also perform peri-anal procedures for things like haemorrhoids, fistulas and fissures and upper and lower GI camera examinations.
My main interest is robotic-assisted surgery and I have helped set up the robotic programme in Northumbria and my previous hospital.
I finished medical school training in 1994 in Manchester returning to my home in the North-East in 2000 to complete my doctorate MD and then start surgical training in 2003.
Mr Harkiran Seehra

I have been in post as a Consultant Colorectal Surgeon at Northumbria since 2003. My formative training was in the North-West and I completed my higher surgical training in the Mersey Deanery. I perform lower GI endoscopy and perform most major colorectal procedures for cancer and benign conditions. My specialist interests are in complex proctology.
Mr Iain McCallum

I was appointed as a consultant surgeon in Northumbria in 2017. I offer most colorectal surgical treatments including bowel resection for cancer and peri-anal procedures for things like haemorrhoids, fistulas and fissures and upper and lower GI endoscopy. I have a special interest in organ-sparing surgical treatment of early rectal cancer and Inflammatory Bowel Disease and over the next year look forward to developing into robotic practice.
I trained in Aberdeen and the North-East and completed a PhD regarding lifestyle risk factors for bowel cancer and their epigenetic mechanisms.
Together with Mr Box, I am the main surgical input for the Inflammatory Bowel Disease Multidisciplinary Team meeting.
Miss Kate Carney

I was appointed as a Consultant Surgeon in Northumbria in 2017. My specialist interests include Early Colorectal Cancers, Transanal Minimally Invasive Surgery, Robotic Surgery and Proctology.
I am the Clinical Lead for the Colorectal Surgery department.
I also have a keen interest in teaching and training, and I am the Postgraduate Lead for Core Surgical Training at the Newcastle Surgical Training Centre.
I am the President of the North-East branch of the Ileostomy Association Patient Support group.
Miss Lena Ngu

I was appointed as a Consultant Surgeon in Northumbria in 2021. I completed my higher surgical training in the North-East. I have completed two fellowships – one at St Marks Hospital in London and a robotic fellowship at Vall d’Hebron Hospital in Barcelona, Spain. I perform most major colorectal procedures for both benign and cancer conditions. I am JAG trained for upper GI and lower GI endoscopy.
My specialist interests include robotic surgery, colorectal cancers, pelvic floor surgery and complex proctology.
Mr Yousif Aawsaj

I finished my higher surgical training in the North East. I have completed a Post CCT Royal College of Surgeons-approved fellowship in robotic and advanced colorectal surgery in Liverpool. I was appointed as a consultant surgeon in Northumbria in September 2023. I offer colorectal surgical services including bowel cancer resection, and most proctology work such as perianal fistula, fissures, and haemorrhoids. I offer and train endoscopic services for both upper and lower GI endoscopies. I am interested in complex benign gynaecological conditions such as endometriosis and often jointly operate with the gynaecology team. I have developed a special interest in the management of complex abdominal wall hernias such as complex incisional hernias, parastomal hernias and other common hernias. I am very keen minimal invasive surgeon, currently doing most colorectal resections robotically. Looking forward to taking this service forward.
I have an MSc degree from the University of Bristol, and I am interested in education and training; I have a Master’s degree in education of health profession.
Miss Susanne Reinoehl

I first joined Northumbria in 2005. After stints working in Africa and on parental leave, I became a SAS doctor attached to the colorectal surgery department in 2012 and have long been interested in promoting and supporting this diverse and growing grade. In April 2024, I was appointed to the SAS Advocate post which is the lead role for the SAS group. I also serve as LNC member and regionally as deputy chair for the BMA Northern Region SAS Committee. Clinically, I work as an independent upper and lower GI endoscopist with a special interest in complex polyps and training. I established the temporal artery biopsy service and am the clinical lead for the trust-wide Lumps and Bumps service.
Mr Samim Al-Zubaidi

I was appointed as consultant colorectal surgeon at Northumbria in 2024. I possess extensive international experience in advanced surgical oncology, emergency general surgery, and colorectal surgery. My career commenced in India, where I completed a three-year training program specialising in managing complex cancer cases, including pelvic exenteration, lateral pelvic side-wall lymph node dissection, and recurrent rectal cancers. Subsequently, I further refined my surgical expertise in Dubai before relocating to the United Kingdom. During my tenure as higher surgical trainee in the North East of England, I specialised in emergency general surgery and colorectal surgery, with a particular focus on robotic colorectal surgery and minimally invasive proctology. Beyond my clinical responsibilities, I am dedicated to advancing surgical knowledge through research. I regularly present at national and international conferences and am equally passionate about education, actively mentoring and training the next generation of surgeons. My leadership abilities are further enhanced by a Master’s in Strategic Leadership in Public Services, which enables me to drive innovation and excellence within healthcare systems.
Mr Charles Johnson

I was appointed as a consultant colorectal surgeon in Northumbria in 2025. Prior to this I completed higher surgical training across the North East of England, then a Royal College of Surgeons Fellowship in robotic colorectal surgery in Sunderland.
I perform minimally invasive major surgery for colorectal cancers, perianal procedures for haemorrhoids, fistulae and fissures, general surgical procedures including hernia repairs, and diagnostic endoscopy.
My specialist interests include robotic surgery, inflammatory bowel disease (IBD) and medical education. I provide surgical input for the IBD service.
The colorectal nursing team is made up of 7 nurses who have all come from a range of backgrounds. They work closely with consultant colorectal surgeons as well as other members of the multidisciplinary team to support you after your diagnosis of cancer.
The role of the team is to offer you support, information and advice from the time of diagnosis, throughout your treatment and follow-up care. The colorectal nurse specialist will act as your point of contact. This means they will be the main person involved in coordinating your care and arranging things for you. They are a consistent point of contact for you, your family and any professionals involved in your care.
The colorectal nurse specialist can help in a variety of ways. They can:
- Support you and your family from the time of diagnosis, throughout your treatment and beyond.
- Advise you on a range of issues related to having cancer.
- Provide written and verbal information about your condition, any investigations and treatments you may need as well as information on wellbeing topics and practical matters.
- Refer you to other healthcare professionals and specialist support services as required.
- Answer your questions and discuss your concerns.
- Signpost you to support groups, health and social care services.
The stoma care nurse specialists are a small but experienced team of 9 specialist nurses offering pre and post-operative support, advice, teaching and practical care to stoma patients within our trust. They see ward patients at NTGH and NSECH and run clinic appointments alongside our phone consultations and home visits.
They aim to support Ostomates on their journey from before surgery and subsequently for as long or often as required as after surgery. If you are preoperative and your surgery is planned, they will meet with you to discuss the implications of stoma formation and provide written information, so you know what to expect.
The specialists will have regular contact with you after your surgery, where they will assist you in learning to look after your stoma. They will see you at home and in the hospital and will support you and your loved ones. They will routinely see all patients in the 12 months following surgery for support. If you are attending a clinic appointment, please bring spare supplies with you as the team will need to remove your pouch.
Outpatient clinics:
- Wansbeck – Weekly on a Monday all-day
- Hexham – Weekly on a Wednesday morning
- Alnwick – First, second & fourth Thursday morning of the month
- Berwick – Third Thursday morning of the month
- NTGH – Weekly on a Friday all-day
Support groups held by other stoma patients in the area
This is a great opportunity for you to meet other people with a stoma and keep up to date with new products.
- Berwick: William Elder Building - held on the third Thursday of the month from 10.00am to 12.00am
- North Tyneside: Diabetic resource centre - held on the first Tuesday of the month from 1.00pm to 3.30pm
- Alnwick: Mind and soul hub - held on the first Thursday of the month from 7.00pm to 8.00pm
- Hexham: Education centre in Hexham General Hospital - held on the first Wednesday of the month from 1.00pm to 2:30pm
Liz Robinson - Lead colorectal clinical endoscopist

I have been working within the speciality of colorectal surgery since 1990. Upon qualifying as a registered nurse, I worked on a busy colorectal ward at the Freeman Hospital in Newcastle. In 1996 I was appointed as a colorectal nurse specialist. This was a dual role caring for patients who had undergone colorectal surgery and stoma formation.
In 2012, I moved to Northumbria to commence a training position as a colorectal nurse endoscopist delivering bi-directional endoscopy.
I was appointed lead colorectal clinical endoscopist in 2020. This role involves undertaking gastroscopy, and colonoscopy and managing the nurse endoscopist, colorectal nurse specialists and stoma nursing team.
I am passionate about the colorectal nursing team delivering outstanding patient care. My role as the lead is to support the nursing team in enhancing their clinical skills, academic studies and to fulfil their career aspirations. I believe this then fosters a motivated, dynamic and enthusiastic nursing team which is highly skilled and patient-focused.
Debbie Sharples - Senior clinical nurse endoscopist

I work as a senior clinical endoscopist within Northumbria and my areas of specialism are particularly in lower GI endoscopy however I do perform upper GI endoscopy too.
I am a very experienced endoscopist and have worked for the trust in my current role for 22 years.
I am responsible for the training of both doctors and nurses in the art of colonoscopy.
I am also the educational lead within the colorectal team and facilitate student placements within this area of specialism.
I perform endoscopy sessions trust-wide and provide clinics for urgent referrals.
Helen Watson - Senior clinical nurse endoscopist

Qualifying in 1987 with a first-class honours degree, Helen works as a senior clinical endoscopist for the trust. Areas of specialism are particularly in lower GI endoscopy.
Helen is a very experienced endoscopist and has worked for the Trust in her current role and specialist area for 22 years.
Responsible for the training of both doctors and nurses in colonoscopy.
She performs endoscopy sessions trust-wide and provides clinics for urgent referrals.
Pam Robson - Senior clinical endoscopist & bowel screening colonoscopist

I initially qualified as a registered nurse at the Cumberland Infirmary at Carlisle in 1998 and since 2002 I have worked for Northumbria Healthcare where I worked in theatres and then endoscopy. Since 2012, I have worked as a colorectal nurse specialist supporting patients from diagnosis to discharge and work closely with colorectal surgeons in Endoscopy, theatres and clinic.
Following training in colonoscopy and flexible sigmoidoscopy, in 2012 I gained accreditation and became an independent level 2 polypectomist.
I was also accredited in 2015 to carry out bowel cancer screening flexible sigmoidoscopy for patients aged 55 in 2015. However, this programme ceased by NHS England in 2020.
In 2019 I gained accreditation to carry out gastroscopies which means patients who require both a gastroscopy and colonoscopy can attend for one appointment.
I also trained in bowel cancer screening colonoscopy and was delighted to achieve accreditation for this in 2021 and now scope for the screening team every week. I now complete level 3 complex polypectomies.
I train trainee colonoscopists and have a weekly training list at Hexham General Hospital.
I offer a flexible sigmoidoscopy service for rectal bleeding, where I assess symptoms and haemorrhoids for possible ligation of haemorrhoids at the time of the test by applying rubber bands.
Twice a week I have a telephone clinic for assessing direct to investigation.
I action my own histology and radiology requests and verify the colorectal polyp surveillance as per our national guidelines.
My supervising consultant is Mr Iain McCallum.
Jes Miles - Senior clinical endoscopist & bowel screening colonoscopist
I am a very experienced clinical endoscopist for Northumbria Trust. I perform endoscopy sessions trust-wide and provide 2WW clinics for urgent referrals.
I am also an accredited bowel screening colonoscopist performing complex polypectomy lists weekly.
I hold a BSc and MSc in colonoscopy. I completed a postgraduate diploma in advanced nursing practice.
I am an independent non-medical prescriber.
I offer a flexible sigmoidoscopy service for rectal bleeding where I assess symptoms and haemorrhoids for possible ligation of haemorrhoids at the time of test.
Hazel Cagayon - Clinical endoscopist

I originally came from the Philippines and started working for the NHS in 2004. I worked in surgical wards where I gained valuable experience. In 2012, I decided to specialise in stoma care nursing and enhanced recovery after surgery (ERAS). From there, I transitioned into the role of a colorectal nurse specialist, a position I held until 2020 when my role expanded to colorectal nurse practitioner.
I hold a degree in Nursing from my home country and a degree in practice development from Northumbria University. I completed a postgraduate certificate in professional practice also from Northumbria University.
I was JAG accredited to perform colonoscopy in 2023 but have been independently performing flexible sigmoidoscopies since 2020. I am currently training to do gastroscopy and doing Master’s level study as part of the course.
I have been an Independent non-medical prescriber since 2022.
I perform lower endoscopy sessions trust-wide and provide 2WW clinics for urgent referrals.
I am currently working on a multi-media project on enhancing patient information throughout their cancer journey.
Trudi Kennair - Clinical endoscopist

I am a clinical endoscopist in a team of 8 nurses who perform various endoscopic procedures.
My main role is to carry out endoscopy lists in colonoscopy and flexible sigmoidoscopy but also to help manage the 2ww LGI referrals from GP in a safe and timely manner.
This includes triaging the referrals and gathering information regarding the patient and indications for referral. I then assess the patients over the telephone and make clinical decisions as to what is the most appropriate investigation in collaboration with the patient’s wishes. I provide a full explanation of the options available and what this entails.
I worked as a sister in the Endoscopy unit for 7 years before joining the Bowel Cancer Screening Programme for 1 year. I then moved to the colorectal team, starting as a colorectal cancer nurse for 2 years while I trained in colonoscopy, before moving over to the CE team. Working in all of these areas has been incredibly beneficial and allowed me to gain a wealth of relevant knowledge and skills to assist me with my job as a Clinical Endoscopist.
I have also carried out master’s level study including becoming an Independent Prescriber this year. There are so many opportunities within my team to learn and develop and also a great supportive team culture.
I have worked for the trust for 15 years and within this time also worked in collaboration with a neighbouring trust which was also a fantastic experience.
Claire Boon - Clinical endoscopist

I started working for Northumbria Healthcare in 2014, having completed my diploma in adult nursing at Northumbria University, whilst working within the Newcastle Hospitals NHS Trust, qualifying in 2007. I obtained my BSc in practice development in 2017.
I completed the HEE accelerated gastroscopy training at level 7 and obtained JAG accreditation for gastroscopy in 2019, now providing two gastroscopy lists per week. I joined the colorectal team in 2022 and I am currently training for colonoscopy accreditation. I have been a non-medical prescriber since 2022.
Included in my timetable are two colorectal clinical nurse endoscopy telephone clinics, assessing patients via the telephone and directing them to the appropriate investigations. Part of my role is also to triage the two-week-wait colorectal referrals.
I am based mainly at Wansbeck Hospital but work trust-wide.
| Name | Secretary to |
|---|---|
| Liz Butcher - Medical secretary | Mr Seehra and Mr McCallum |
| Susan Kitching - Medical secretary | Mr Hicks and Miss Carney |
| Kate Langers - Medical secretary | Mr Box and Mr Kelly |
| Beverley Davies - Medical secretary | Mr Emmet and Miss Ngu |
| Victoria David - Relief medical secretary | Mr O'Dair and Mr Aawsaj |
| Suzanne Hawksby-Rogerson - Relief medical secretary | CNS and stoma team |
| Bethany Hodgson | Transcriptionist |
| Hilary Sked | Transcriptionist |
Colorectal cancer patient journey
If you are being seen for colorectal cancer, this interactive document helps you explore the steps in your cancer journey.
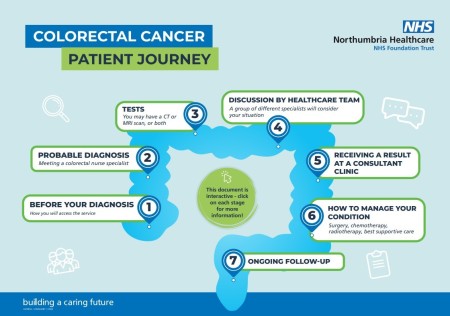
You can also read about the different steps below and watch our video about your cancer journey.
You will be referred to us if:
Your GP has referred you on a faster diagnosis pathway. This is because you have symptoms that may indicate you have bowel cancer. You will have had either a colonoscopy, CT scan or both to confirm this.
A consultant has seen you to assess your symptoms.
You may have taken part in the national bowel cancer screening programme.
More information is available on our endoscopy page.
Following a probable
You will also have a blood test, so they can see if you're anaemic. If you are found to be anaemic, you may require an Iron infusion. You will receive more detail if this applies to you.
Our cancer prehabilitation team will also contact you. They help you get in the right condition for treatment. For more, visit our cancer prehabilitation pages.
When we have all the results from your tissue samples and scans, our team will discuss treatment options.
Our team includes doctors, nurses, coordinators, radiographers and pathologists.
After our meeting, you will be 
You will discuss the outcome of the meeting and your treatment options. We will make sure you fully understand the options before you agree to any treatment.
Your treatment options will depend on many factors. This includes:
- Where the cancer is in the bowel
- Whether it has spread to other parts of your body
- Your general health and fitness
- Any other significant health problems that you may have
- What you want
Your healthcare team will be there to support you, and your family. They will answer any questions that you may have.
More information on treatment is available here.
After your treatment, you will attend our nurse-led clinics.
This may be to make sure that the cancer has not come back or spread. You may need help to manage your symptoms.
We can also refer you to other services within the community. These can help and support you and your family.
Other resources:
Cancer information and support: Cancer information and support :: Northumbria Healthcare NHS Foundation Trust
Living well and beyond cancer: Living well | Our publications | Bowel Cancer UK
Stratified follow-up pathway: Living with and beyond cancer - Northern Cancer Alliance
Follow-up care after treatment: Follow-up care after treatment | Macmillan Cancer Support
Useful links
The below QR code poster has links to support and information you may find useful.
The links are also listed below.

About bowel cancer - https://
Live Well with Cancer - https:/
Diagnosis - https://
Early diagnosis- https://
Living with and beyond bowel cancer- https://
Lynch syndrome- https://
Macmillan benefits and financial support- https://
Maggie’s Centre- https://
Never Too Young- https://
Preparing for surgery- https://
Types of surgery- https://
Video consultations
We can offer online consultations where appropriate via a video call to make it easier for you to attend.
Rather than travelling to your appointment, you will receive a text or email before your appointment and simply need to click to join. Find out more here.
