Our urology department offers a modern service, built around your needs. Our vision is to provide high-quality and safe care for our communities.
Urologists treat conditions affecting the bladder, kidneys and prostate. This includes incontinence (loss of bladder control), impotence, and cancer.
Our service is growing. We have recruited more staff and we have more equipment and facilities. We review our pathways regularly to improve services for our patients.
About our service
You may be referred to us if you have:
- Blood in your urine
- Blood in your semen
- Pain in your side suggesting kidney stones
- Urinary tract infection
- Erectile dysfunction
- Tight foreskin
- Raised count from a prostate blood test (PSA)
- A lump in your testicle
You can read more about these symptoms here.
We have both consultant and nurse-led clinics.
For your condition, we may have specialist nurses who can support your care. You may need tests before seeing a clinician later to agree a treatment plan.
You may be offered a phone appointment. A clinician will call you to talk about your issue. This call will be from a private number. The clinician may not be able to stick to your appointment time exactly.
For some specialist clinics and treatments, you may need to limit what you drink beforehand.
For ultrasound and some other scans, you may need to hold urine (wee) in your bladder.
For many of our appointments you may need to give a urine (wee) sample when you come.
Your appointment letter or information leaflet will explain more about this.
Urology Day Unit, Wansbeck General Hospital
Urology Day Unit, North Tyneside General Hospital
Endoscopy Unit, Hexham General Hospital
Switchboard: 0344 811 8111
Urology clinic: 01670 529314
Appointment line: 0191 203 1212
Urology specialist nurses' secretary: 01670 529129
Conditions
This clinic is to find out why you have blood in your urine (wee). You may have spotted it yourself. A GP may have detected it through a test.
After your referral, you may get appointments for:
- An ultrasound or CT IVU (intravenous urogram) scan
- Flexible cystoscopy - a flexible camera to look at the lining of your bladder. This will take place under local anaesthetic.
The order of these tests may change.
You may get a text message before coming to your appointment.
Kidney stones are usually found in the kidneys or in the ureter, the tube that connects the kidneys to your bladder. They can be extremely painful. They can lead to kidney infections or the kidney not working properly if left untreated.
If your kidney stones are too big to be passed naturally, they're usually removed by surgery.
More information is available here.
Bladder cancer is the second most common urological cancer after prostate cancer. It is more common in men. Around 10,000 people are diagnosed with bladder cancer each year.
The main risk factor for bladder cancer is smoking. However, certain jobs or occupations put people at risk of getting a bladder tumour.
We carry out different tests to diagnose bladder cancer. They include:
- A CT scan of your kidneys and bladder
- An ultrasound scan of your kidneys and bladder
- Using a flexible camera to look at the lining of your bladder (cystoscope). This takes place under local anaesthetic.
Treatments
Treatments include:
- TURBT - transurethral resection of bladder tumour
- BCG
- Mitomycin C
- Treatment for more advanced bladder cancer
- TULA
You can find out more about them here.
Patient journey
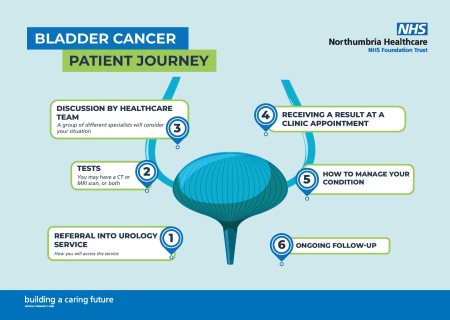
1. Referral
You will be referred to us if:
Your GP has referred you on a faster diagnosis pathway. This is because you have symptoms that may indicate you have bladder cancer and need further investigations.
The urology team will be in contact you within 2 days. The clinician will discuss your symptoms and may arrange further tests.
2. Tests
You will have diagnostic tests in the form of CT scan and flexible cystoscopy. Information on these tests is further down on this page.
This will help you and your doctor to decide what treatment will be best for you.
3. Discussion by healthcare team
When we have all the results from your tests, our team will discuss treatment options.
Our team includes doctors, nurses, co-ordinators, radiographers, pathologists.
4. Receiving a result at a clinic appointment
After our meeting, you will be invited to attend a clinic. You will see a member of the urology clinical team. This will usually be within 1 week of the team meeting.
Cancer prehabilitation is available for all patients. Find out more here.
5. How to manage your condition
Your treatment options will depend on many factors:
- Where the cancer is within your bladder
- Whether it has spread to other parts of your body
- Your general health and fitness
- Any other significant health problems that you may have
- What you want
- Active surveillance (being closely monitored by regular checks)
Your healthcare team will be there to support you, and your family. They will answer any questions that you may have.
https://
7. Ongoing follow-up
After your treatment, you will attend our nurse-led clinics.
This may be to make sure that the cancer has not come back or spread. You may need help to manage your symptoms.
We can also refer you to other services within the community. These can help and support you and your family.
Supporting you
Cancer can affect every aspect of your life and those around you. We know it can be a difficult and frightening time for you and your loved ones. We have put together this webpage to help you live with and beyond cancer - Cancer information and support :: Northumbria Healthcare NHS Foundation Trust
Macmillan Cancer Support
Macmillan has an excellent package of advice. This can help you and your loved ones manage the impact of cancer. This could be:
- Support for financial worries
- Online events
- Programmes to help with your overall health and wellbeing
For help, or if you need someone to talk to, call 0800 808 00 00 or visit theMacmillan website.
The kidneys are two fist-sized organs on either side of the body. They sit just under the ribcage. Their main role is to filter out waste and excess water from the blood, producing urine (wee).
Kidney cancer tends to affect people in their 60s and 70s. It may be found when investigating other conditions. This means it is often in the early stages and so easy to manage. Symptoms of kidney cancer include blood in your urine (wee), pain or a mass (bulge) in the stomach area.
If you do have a lump in the kidney, we will need to do some tests. We will then talk to you about the different types of treatment.
We will first need to check if the cancer is localised to the kidney or if it has spread anywhere else this is done using a CT scan and may also necessitate a bone scan if the tumour is very large.
Treatment
Treatments include:
- Monitoring
- Microwave ablation
- Removing a kidney (nephrectomy)
- Removing the cancer but leaving as much of the kidney as possible (partial nephrectomy)
You can find out more about them here.
Supporting you
Cancer can affect every aspect of your life and those around you. We know it can be a difficult and frightening time for you and your loved ones. We have put together this webpage to help you live with and beyond cancer - Cancer information and support :: Northumbria Healthcare NHS Foundation Trust
Macmillan Cancer Support
Macmillan has an excellent package of advice. This can help you and your loved ones manage the impact of cancer. This could be:
- Support for financial worries
- Online events
- Programmes to help with your overall health and wellbeing
For help, or if you need someone to talk to, call
The prostate is only found in men. It sits just outside the bladder around the urethra (waterpipe). This is why some men with prostate issues have trouble passing urine (weeing). The prostate produces some of the liquid for the sperm as ejaculation occurs.
Prostate cancer is the most common male cancer. There is no screening test yet. If you have concerns, please make an appointment to see your GP. To check your risk, the doctor will look at your prostate and you may need a blood test. This is known as a PSA.
If you are referred to us, a member of the team will talk to you about your symptoms and any other medical problems. They will repeat the examination of the prostate gland.
The doctor or specialist nurse will talk about the tests needed to check you for prostate cancer. This may include an MRI scan to highlight any abnormal areas You may need a prostate biopsy. For this, you may need a local or short general anaesthetic.
We will see you in clinic to talk about the results. You may need some further scans to help the doctors decide the best treatment. We will talk about all the treatment options with you.
You can find out more about the different tests and scans used to diagnose prostate cancer here.
Treatment
The treatment you can have is affected by:
- How aggressive the cancer is
- Whether it is only in the prostate)
- Any other medical problems you may have now or have had in the past
Options include:
- Monitoring
- Radical prostatectomy (surgical removal of your prostate gland)
- Hormone treatment
You can find out more about them here.
Patient journey
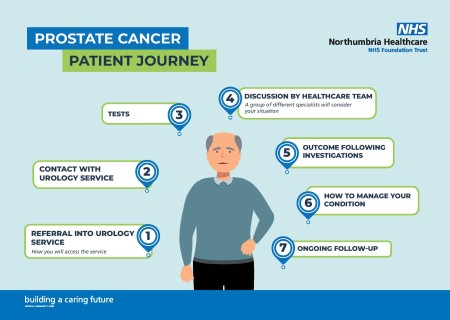
1. Referral
You will be referred to us if:
Your GP has referred you on a faster diagnosis pathway. This is because you have symptoms that may indicate you have prostate cancer and need further investigations.
The urology team will be in contact you within 2 days. The clinician will discuss your symptoms and may arrange further tests.
2. Contact with urology service
The nurse specialist will contact you. They will introduce themselves and explain your patient pathway and their role in this. You will receive their contact details at this stage.
3. Tests
You will have diagnostic tests in the form of MRI, CT scan, TP biopsy, bone scan, PET (you may not need all of the above). Information on these tests is further down on this page.
This will help you and your doctor to decide what treatment will be best for you.
https://
4. Discussion by healthcare team
When we have all the results from your tests, our team will discuss treatment options.
Our team includes doctors, nurses, co-ordinators, radiographers, pathologists.
5. Outcome following investigations
After our meeting, you will be invited to attend a clinic. You will see a member of the urology clinical team. This will usually be within 1 week of the team meeting.
Cancer prehabilitation is available for all patients. Find out more here.
6. How to manage your condition
Your treatment options will depend on many factors:
- Where the cancer is within your prostate
- Whether it has spread to other parts of your body
- Your general health and fitness
- Any other significant health problems that you may have
- What you want
Your healthcare team will be there to support you, and your family. They will answer any questions that you may have.
https://
7. Ongoing follow-up
After your treatment, you will attend our nurse-led clinics.
This may be to make sure that the cancer has not come back or spread. You may need help to manage your symptoms.
We can also refer you to other services within the community. These can help and support you and your family.
Supporting you
Cancer can affect every aspect of your life and those around you. We know it can be a difficult and frightening time for you and your loved ones. We have put together this webpage to help you live with and beyond cancer - Cancer information and support :: Northumbria Healthcare NHS Foundation Trust
Macmillan Cancer Support
Macmillan has an excellent package of advice. This can help you and your loved ones manage the impact of cancer. This could be:
- Support for financial worries
- Online events
- Programmes to help with your overall health and wellbeing
For help, or if you need someone to talk to, call
After your GP refers you, we may send you for tests before seeing the team.
Our specialist nurses may care for you. They will assess you over a much longer appointment time.
They will talk to you about things you can do to help. This includes changing what you eat, checking how much you drink, advising on pelvic floor exercises.
Erectile dysfunction (ED), also known as impotence, is the inability to get and maintain an erection.
Erection problems (dysfunction or impotence) are common in men as they get older. You are not alone. Half of all men between 40 and 70 are estimated to have it to some degree.
There are a range of options available to treat it or improve the quality of erections.
The simplest treatment is medication. This works in up to 70% of men. If tablets do not work or are not suitable for you, there are other options.
We offer surgery to correct penile curvature (including Peyronie’s disease).
We know that these conditions can be sensitive and very distressing. Our staff are committed to treating you with the utmost dignity and sensitivity. They will give you with the highest quality of care in a safe and comfortable environment.
Tests and procedures
Scans
Bone scan (BS)
A bone scan is an imaging test. It uses a very small amount of radioactive dye to help diagnose problems with your bones.
MRI
An MRI scan uses a powerful magnet and radio waves to scan your body. It gives us detailed images of your prostate gland.
PET
A PET scan uses low-dose radiation to measure the activity of cells of different parts of the body.
CT
A CT scan takes a series of x-rays which build up a 3D picture of the inside of the body.
More about tests, procedures and scans is available here.
Video consultations
We can offer online consultations where appropriate via a video call to make it easier for you to attend.
Rather than travelling to your appointment, you will receive a text or email before your appointment and simply need to click to join. Find out more here.
