A nasendosocpy assessment aims to identify if anything in your throat is causing, or contributing to symptoms of throat irritation, coughing, breathlessness, voice changes, and/or swallowing difficulties.
A nasendoscopy is a thin flexible tube with a camera at the end. It helps health professionals to get a closer look at the inside of your
- Nose
- Throat (pharynx)
- Voice box (larynx)
The nasendoscopy assessment is carried out in an outpatient clinic of surgical day unit.
We have routine clinics in North Tyneside General Hospital and Wansbeck General Hospital. We hope to develop ‘out-reach’ nasendoscopy clinics in Alnwick and Hexham. We can also carry out these assessments on hospital wards.
The results of the nasendoscopy helps health professionals to better understand what could be causing your symptoms, and in turn how to manage them.
More specifically, nasendoscopy results give us information about:
- How healthy your throat and vocal cords are.
- How the muscles in your throat are moving.
- Whether you would benefit from specific throat care recommendations.
- Whether breathing, or cough control exercises could be helpful for you, and if so, which ones would be most helpful
- Whether voice or swallowing exercises, or diet modifications would be helpful for you.
There are no special preparations for the nasendoscopy.
You can eat, drink, and take medication as normal, and drive before and after the procedure.
A Speech and Language therapist (SLT) will perform the assessment, with support from another SLT or an SLT assistant.
- You will be awake, sitting down and able to speak during the assessment.
- A thin flexible tube will be passed through your nose.
- The tube only goes in about 3-4 inches.
- Once in place, the tube sits just behind your nose and looks down at your throat.
- The tube does not go into your windpipe and should not make it difficult to breathe.
- We will ask you to perform some breathing and speaking tasks (e.g., counting from 1-5) and may try to trigger your symptoms if you are happy for this.
- We will practice some breathing and/ or ‘cough- control’ exercises to see if they can help you to control of your throat muscles
- If you have reported swallowing difficulties, we might give you something to eat and/or drink whilst the camera is in place
-
If you have reported voice difficulties, we might try some voice exercises whilst the camera is in place.
Most people tolerate the examination extremely well and often report that it wasn’t as bad as expected. You can ask the SLT to stop the assessment at any point.
The whole appointment typically lasts about 30 minutes.
The nasendoscopy procedure itself should only last about 5 minutes.
There will be time before and after the procedure for questions, feedback, and discussion.
The video-images of the assessment are recorded. We can show you these in the session with an explanation of what they mean for your diagnosis and treatment plan. Here is an example of what vocal cords look like during a nasendoscopy assessment:
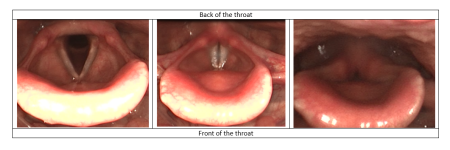
This is the kind of image that the health professional will see when they do the nasendoscopy assessment. These images show the inside of your throat, more specifically your ‘voice box’.
The two white lines are the vocal cords, they sit horizontally in our throat, behind the adam’s apple. They open and close to co-ordinate breathing, voicing, airway projection during swallowing, and coughing.
Picture 1 – The vocal cords are open (in a v-shape) so we can breathe air in and out of the windpipe, which leads down to the lungs
Picture 2 – The vocal cords come together gently and vibrate to produce voice.
Picture 3 – The vocal cords squeeze tightly together to ‘hold the breath’ and build up pressure behind a cough e.g. when removing unwanted material from the airway(wind-pipe)
Most patients find the information from this examination helpful for understanding their symptoms.
Findings help the SLTs to develop a personalised care plan which aims to help you to control your throat symptoms more effectively.
For most people, this is a very low-risk procedure. The most common risk is mild discomfort. If experienced, this tends to be when passing the scope through the nose but this discomfort eases once the nasendoscope is in place. Some people describe this as an ‘extreme tickle’.
There are also reports of a small number of people experiencing:
- A nosebleed (epistaxis): This risk is higher for people on antiplatelet therapy, thrombolysis, aspirin medications, or who have had previous trauma to the inner lining of the nose.
- Gagging: This risk is higher for people with a known strong gag reflex. In extreme cases this can lead to vomiting.
- A fainting (vasovagal) episode: This risk is higher for people with a history of fainting, including people with an unstable cardiac status, or those feeling very anxious about the procedure.
- An allergic response to topical anaesthesia: We tend to avoid using topical anaesthesia for respiratory assessments as this will affect the outcome of your assessment but on the rare occasion that it is used, your SLT will check whether you have any known allergies. The most used topical anaesthesia is Lidocane.
If you feel any of these could be a risk for you, please discuss this with your SLT before, or at the beginning of your appointment.
Yes. Your SLT is trained in techniques to make the procedure as safe and comfortable as possible. This can include trying different sitting and/or head postures, using extra lubrication for the nasendoscope, and in some cases, using nasal decongestants to open the nasal passages. Breathing techniques can be used help to reduce irritation in the nose and throat.
For people with confirmed severe lower airways disease e.g., asthma we may avoid using aerosol sprays. We will still be able to get valuable information from looking at your throat and observing what happens when you are breathing at rest and talking.
Your SLT will always be led by you. If you want them to stop at any point, you can ask, and they will stop the procedure.
If you are having a flare-up of your asthma, or have a virus or infection, we will most likely delay the procedure.
If you have asthma, you should always bring your reliever inhaler to this appointment e.g. Ventolin (blue inhaler).
The risks vs benefits will be weighed up for all patients. The main patient groups that we would consider most at risk of complications would be those who have:
- Skull base/ facial surgery or fracture, in the last 6 weeks
- Major or life-threatening nosebleeds (epistaxis), in the last 6 weeks
- Trauma to the nose due to injury or surgery, in the last 6 weeks
- Sino-nasal and anterior (front) skull base tumours/ surgery
- Nasopharyngeal stenosis
- Craniofacial abnormalities
- Hereditary haemorrhagic telangiectasia (an inherited genetic disorder that affects blood vessels)
- Choanal atresia (a rare condition that is present from birth, where nasal passages are blocked by bone or tissue)
- Laryngectomy within the previous two weeks
We politely request that if you are experiencing a chest infection or virus, that you contact us to reschedule your appointment.
